Full mouth dental implants offer a transformative solution for many adults coping with extensive tooth loss, restoring appearance, chewing ability, speech, and self-assurance. Choosing this procedure is a big step that demands research and self-reflection about individual needs and readiness. Online resources often detail the steps involved, helping potential patients see the big picture and the finer details. Still, a personal, informed decision goes beyond any single webpage—it combines professional guidance, trusted educational materials, and careful consideration of one’s unique circumstances.
What Are Full Mouth Dental Implants?
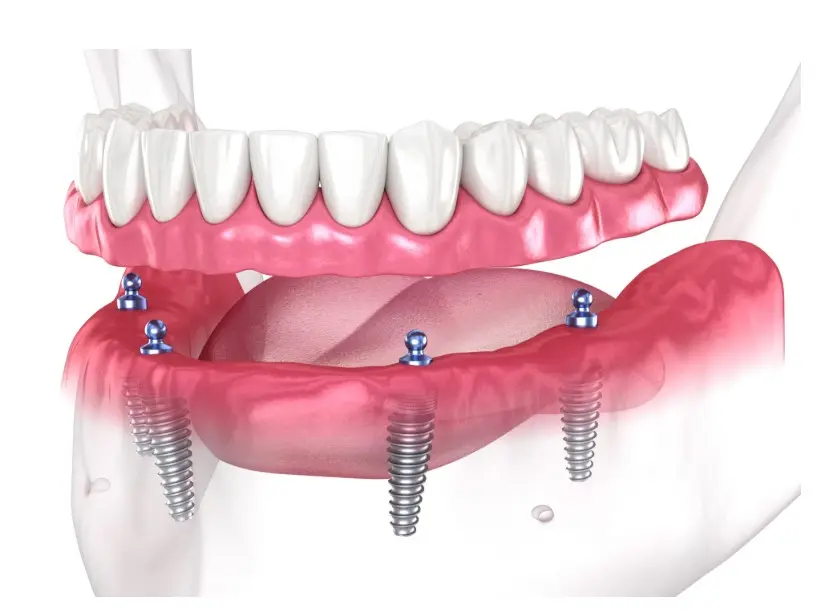
Full mouth dental implants are a comprehensive solution for individuals who have lost most or all of their teeth. Unlike removable dentures, this method uses multiple implants placed in the jawbone to support a complete set of fixed prosthetic teeth. The goal is to restore function, aesthetics, and oral health by mimicking the structure and stability of natural teeth. Those seeking a long-term alternative to traditional dentures and bridges often choose this approach, especially when jawbone preservation is a concern.
The process typically involves an initial assessment, implant placement, healing time, and attachment of the final prosthetic. Each step is carefully planned to ensure comfort, functionality and lasting results. For those seeking clarity on the procedure, www.ora4x.com/dental-implants/full-mouth-dental-implants/ offers detailed insights into what full mouth dental implants involve, from consultation to recovery. Reviewing such resources can support informed decision-making and set realistic expectations for anyone considering this treatment.
Who Is a Candidate?
Deciding who qualifies for full mouth dental implants involves a careful and customized assessment. Dentists look first at the health and density of the jawbone, as the bone must be strong enough to anchor the titanium posts. Through 3D imaging and scans, specialists measure bone quality and identify any need for bone grafting in patients with significant bone loss. Candidates also need to be free from active oral infections and have healthy gums, as these conditions can impact the success of implant integration.
General health is equally significant. People with well-controlled chronic illnesses, such as diabetes or hypertension, can often undergo implant placement with minimal risk, provided they collaborate closely with their healthcare teams. On the other hand, those who smoke heavily, suffer from autoimmune disorders, or are on medications that affect bone healing may require special consideration and additional preparation. Commitment is another factor—candidates must be willing to practice daily oral care, attend regular professional cleanings, and heed post-surgical instructions to ensure their investment lasts.
Benefits of Full Mouth Implants
The rewards of full mouth implants can be seen in daily functionality and felt in emotional well-being. The most immediate benefit is restored chewing ability; implant-supported teeth allow most patients to return to a normal, unrestricted diet. There is no longer any worry about teeth slipping or falling out while speaking, laughing, or eating, which means greater spontaneity in social interactions and improved speech clarity. Beyond function, the confidence from a stable, natural-looking set of teeth can be life-changing. Full mouth implant patients often express a shared sentiment: they feel younger, healthier, and eager to smile. Psychologically, data indicate reduced social anxiety and a better quality of life. Health-wise, implants slow bone loss in the jaw—a common issue when teeth are missing—and support adjacent structures, helping to maintain a fuller and more youthful appearance. Additionally, since implants don’t depend on the support of other teeth, remaining healthy teeth aren’t compromised, making this option more conservative in some respects compared to fixed dental bridges.
Potential Risks and Challenges
No surgical procedure is without risk. Dental implant placement may cause temporary swelling, bruising, or minor bleeding in the first days following surgery. More rarely, complications such as infection, injury to surrounding nerves, or sinus problems (particularly when working with upper jaw implants) can occur. The success rate remains high, especially with skilled providers and good patient cooperation.
On the practical side, the financial investment is often the most significant hurdle for patients. Cost depends on the number of implants required, the complexity of each case, the materials chosen for the prosthetics, and additional treatments like bone grafts or sinus lifts. The time commitment also warrants attention—multiple visits, healing periods, and the need for ongoing maintenance mean this isn’t an overnight transformation. Still, the benefits significantly outweigh the drawbacks for most individuals who meet the health prerequisites and are motivated to sustain their results.
The Implant Process: Step-by-Step
1. Consultation and Evaluation
The journey starts with a thorough evaluation. A dentist or oral surgeon will review your medical and dental histories, take digital scans or X-rays, and craft a personalized treatment plan. This visit is your chance to ask about expected results, timelines, and any pre-treatment steps—such as tooth extractions or bone augmentation—that may be required.
2. Treatment Planning
Using diagnostic data, your team maps out how many implants are needed and where they’ll be placed for optimal support. Some patients receive computer-guided surgery plans for added accuracy, particularly in complex cases.
3. Implant Placement Surgery
Usually performed under local anesthesia, surgical placement is relatively straightforward for most. Aftercare instructions will address diet, hygiene, and managing discomfort. Healing—known as osseointegration—takes several months as the bone gradually fuses to the implants. During this phase, temporary restorations may be worn so you never have teeth.
4. Restoration and Finalization
Once healing is complete, abutments and the custom-made prosthetic are attached. Your smile is restored, function returns, and you enter the maintenance phase. Most patients find adapting to their new teeth surprisingly quick, though regular dental visits remain essential for long-term success.
Considering Cost and Alternatives
Cost is an essential factor that should be discussed openly with your provider. Full mouth dental implants often involve a significant financial commitment due to the complex laboratory work, high-quality biomaterials, and several appointments required. Insurance coverage may be limited and usually only covers the surgical aspect, not the final teeth. Inquiring about office payment plans or third-party financing options is advisable to make the overall timeline and costs more manageable.
Alternative treatments—including removable partials, implant-supported dentures, or fixed bridges—might offer more affordable or less invasive options. However, they may not provide a complete implant solution’s stability, bone support, or longevity. Balancing the upfront and long-term costs, practical benefits, and personal priorities is crucial when selecting the right approach.
Also Read-Longevity Supplements: Enhancing Healthspan and Lifespan through Science